I. How did it all begin?
Although the legal precedence for inclusion can be traced back to Brown v. Board of Education (347 U.S. 483 [1954]), it was really the parent's of children with a disability that encouraged legislators to adopt the Education for All Handicapped Children Act (EAHCA) (PL 94-142) in 1975 which required school district's to both include and educate children with special needs as well as to create specialized academic plan (later to be known as an individualized education program or IEP) for them.
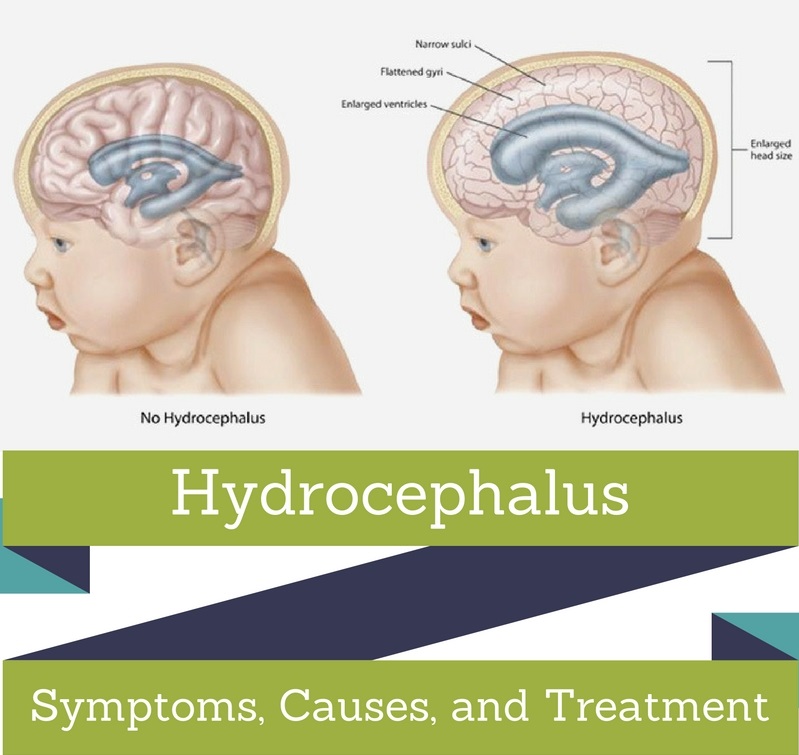
Because of its honorable beginnings, it only makes sense that the IEP (sometimes also referred to Individualized Education Plan) process was intended to be centered on the student. That being said, which students qualify for an IEP? Below is a listing of the disabilities or impairments that are eligible for an IEP: Autism, Deaf-blindness, Deafness, Emotional disturbance, Hearing impairment, Intellectual disability, Multiple disabilities, Orthopedic impairment, Other health impairment, Specific learning disability, Speech or language impairment, Traumatic brain injury and Visual impairment.
For a parent, it is very simple if you believe that your child is qualified to receive special education services. It's just a matter of going to their teacher, principal, or the school's psychologist. Once you have asked about you child being evaluated for an IEP , a group of qualified personnel (including those outlined above) will decide whether or not an evaluation is warranted and create an appropriate plan if an IEP is deemed necessary. From the time the parent gives consent to proceed with the evaluation, the district has sixty (60) days to complete the evaluation. Any decision regarding the IEP evaluation must, by law, include parental input.
It should be noted that a child's teacher can also refer students for evaluation, but only after attempts have been made to remedy the problem without special education services. If such attempts have been made (and the student is continuing to struggle), the next step is initiation of an intervention under RTI (response to intervention) or convening the school's student services team (SST) to discuss their performance. In this meeting, the general education teacher brings samples of the student's work as well as supportive data such as reading scores and math scores, behavioral charts, and writing samples. From this data, the team can decide whether the student would benefit from an evaluation, or if they should continue without special education services.
If the suspected cause of the problem is the result of a learning or behavioral impairment, the SST can work together to determine what tests need to be done and what data needs to be gathered. This can include a variety of performance-based tests such as Woodcock Johnson, Third Edition (WJIII), or the Wechsler Individual Achievement Test (WIAT). In addition, they might perform cognitive function and behavioral function testing.
Following this testing (and gathering of existing information), the evaluation team will meet again to discuss the results of the tests. At this time, if a decision is made regarding evaluation, the student's parent(s) are invited to participate.
I would be amiss if I did not include the caveat that there are certain diagnosis that neither teachers or school psychologist are not qualified to make. These include Attention Deficit Hyperactivity Disorder (ADHD), Autism (or Autism Spectrum Disorder), as well as most physical and developmental delays require a medical diagnosis. If you are an educator and suspect that you have a student affected by one of these conditions, it is imperative to include a medical professional in the evaluation process.
To sum up this portion of the IEP process, in each category of disability, there must be an impact on the student's education that is directly attributable to the disability and they must be deemed in need of specially designed instruction. After all, not all children with a disability require special education services.
For additional information: Individualized education program (IEP), Summary of PL 94-142