Don't laugh at me (Mark Wills)
Dedicated to my long-time friend Shirley Forry for providing me with the inspiration for this blog.
I. The emotional toll of hydrocephalus
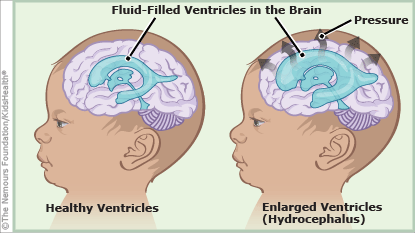
As I prepare to leave for Washington, D.C. on September 11th, I have been challenged by the Hydrocephalus Association (HA) to update my hydrocephalus education and awareness blog as often as possible. Having survived the condition unshunted for 53+ years, I have no shortage of information that I can share, but I wanted to do at least one blog that looks at the emotional toll it takes on those affected by the condition. For most of us - myself included - that would be the cruel and hurtful remarks made by some people. Why is this? Simply put, we live in a society that promotes a narrow standard for attractiveness. Take the images at the top-right and mid-left side of this blog. Most people (especially other children) would look at the image of the me and go "eww". By comparison, the would look at the image of the "normal child" and say nothing. Why is this? According to one author it's because "Digitally altered faces and bodies - beautiful, yet unrealistic - become imprinted in our minds as normative. Anyone outside the bell curve is a potential victim of bullying".
II. How do people with hydrocephalus look?
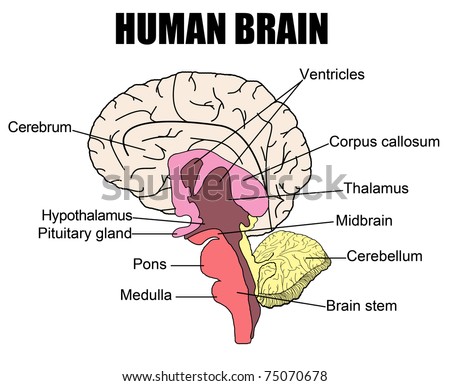
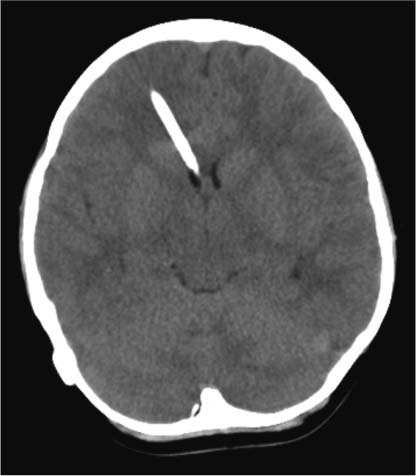
 Perhaps the most noticeable characteristic of people with hydrocephalus (or, at least, those without a shunt) is a larger than normal skull. Take my head for example, it is 9 7/8 inches in circumference. Over the years - I am 53 now - I have been made fun of, teased, and even told that I was "evil" because of how my head looks. The sad part is that it doesn't look any different than an "average" head, just larger. In addition to a larger-than-normal head, many children with hydrocephalus also suffer from "sun-setting" eyes. This condition involves an upward gaze paresis (weakness) while the eye itself appears driven down. It occurs in approximately forty percent (40%) of children with obstructive hydrocephalus and thirteen percent (13%) of children with shunt dysfunction. Although it doesn't have a direct correlation, many people have seen my head and assume that I am developmentally delayed (I will not use the "R" word). According to HA, while developmental disabilities are a possibility, the more frequent problem is the development of social skills -- something I have never had a problem with.
Perhaps the most noticeable characteristic of people with hydrocephalus (or, at least, those without a shunt) is a larger than normal skull. Take my head for example, it is 9 7/8 inches in circumference. Over the years - I am 53 now - I have been made fun of, teased, and even told that I was "evil" because of how my head looks. The sad part is that it doesn't look any different than an "average" head, just larger. In addition to a larger-than-normal head, many children with hydrocephalus also suffer from "sun-setting" eyes. This condition involves an upward gaze paresis (weakness) while the eye itself appears driven down. It occurs in approximately forty percent (40%) of children with obstructive hydrocephalus and thirteen percent (13%) of children with shunt dysfunction. Although it doesn't have a direct correlation, many people have seen my head and assume that I am developmentally delayed (I will not use the "R" word). According to HA, while developmental disabilities are a possibility, the more frequent problem is the development of social skills -- something I have never had a problem with.III. Conclusion
What can be done for what amounts to bullying? Parents need to teach their children that it is imperative that they treat ALL people with both respect and kindness. They should learn that so-called norms depend upon context and that they will vary from one family to another and, on a larger scale, from one culture to another and ARE NOT based on the air-brushed ideals propagated by the media. Even more importantly it is incumbent upon us, as adults, to remind children that human beings everywhere are interesting and memorable because of - not in spite of - their unique real features.
For additional information: About hydrocephalus, Social skill development in children with hydrocephalus, Sunset eye sign Teased about your looks? Bullying that goes under the radar